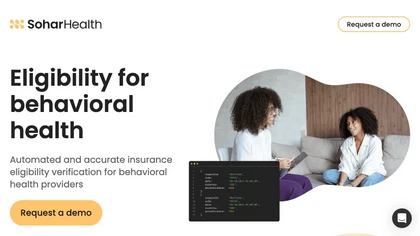
Sohar Health: Streamlining Insurance Eligibility Verification for Behavioral Health Providers
Sohar Health is an AI-powered tool designed to automate and streamline insurance eligibility verification for behavioral health providers. By reducing manual operations and improving team efficiency, this tool allows providers to deliver better outcomes for their patients.
Sohar Health’s impressive accuracy level of 99% automatically verifies eligibility and coverage across hundreds of insurance providers. This helps increase patient intake, conversion rates, and revenue while reducing preventable claim denials.
The tool is integrated with EHR/practice management solutions, providing a seamless workflow. Developers can also benefit from powerful and easy-to-use APIs, ensuring a faster implementation process. Access to comprehensive API documentation, libraries, and technical support is also available.
Backed by leading investors in the industry, Sohar Health is the solution for providers looking to decrease claims denials and understand their patients’ benefits more effectively. Contact Sohar Health today to learn more.
Real Use Case:
Imagine a behavioral health provider who manually verifies insurance eligibility and coverage for each patient. This process can take hours, leading to delays and potential errors in patient care. By using Sohar Health, the provider can automate the verification process, saving time and ensuring accurate information. This allows the provider to focus on delivering quality care to their patients, resulting in better outcomes and increased revenue.